Diabetes and Belonging
Is it true that belonging interrupts six types of stigma in diabetes care?
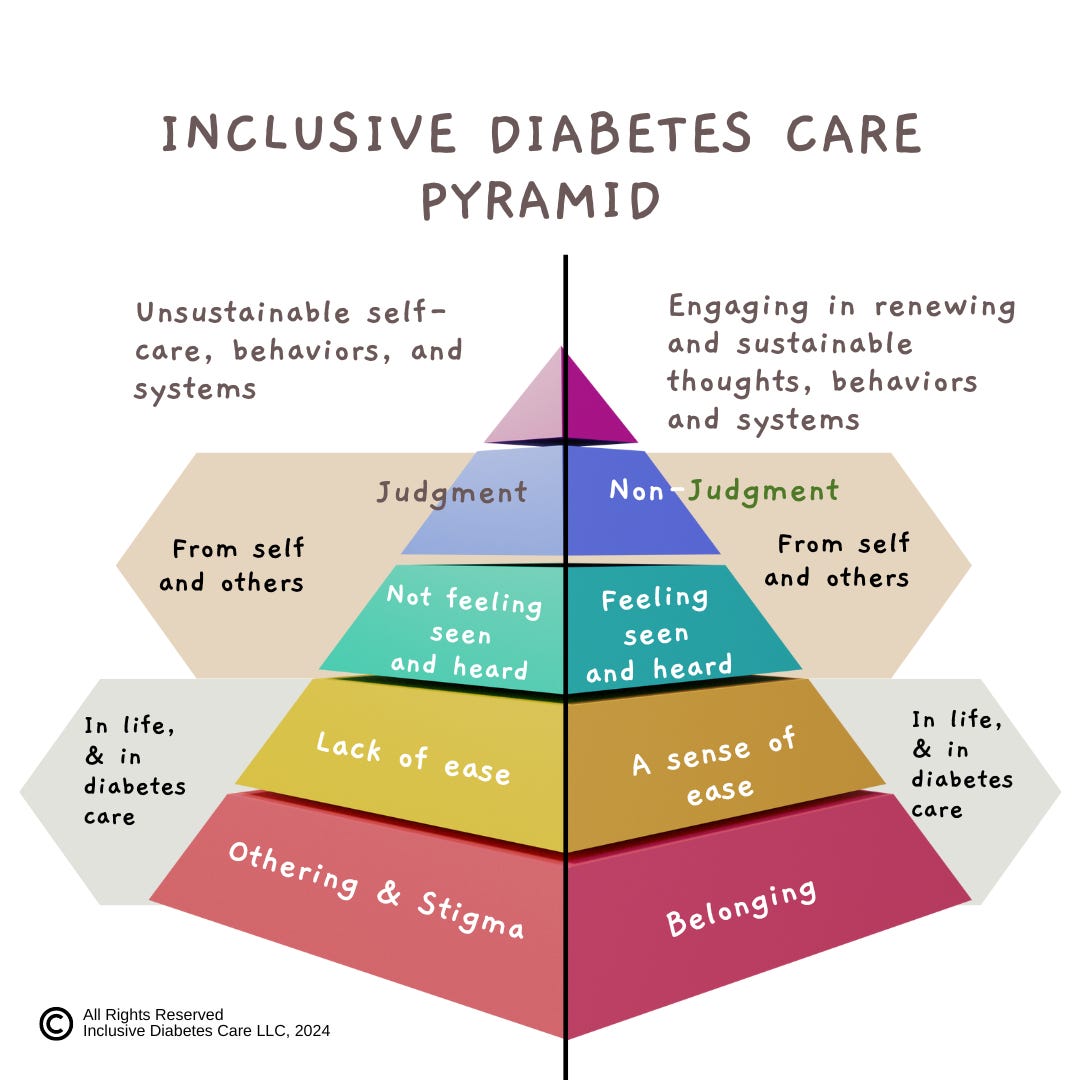
The Inclusive Diabetes Care Pyramid is a visual representation and transformative tool that empowers healthcare professionals to see the profound impact of inclusion and belonging in diabetes care. This article explains how belonging interrupts six types of stigma and how to use the IDC Pyramid within institutions or individual counseling sessions.
The IDC created both an Othering and Belonging Pyramid. This graphic can be used to interrupt the many forms of stigma in diabetes care. To begin, it is important to see that traditional efforts to promote inclusion create groups that are Othered. Seeing how belonging by stigmatizing other groups is not inclusion takes effort. When this happens, the cycle of stigma and othering shifts to another group, which halts effective conversations. For example, if efforts to reduce diabetes result in Othering fat, queer, or financially limited folks who are affected by diabetes, we are not reducing stigma but simply repeating Othering. This concept of belonging without othering is the goal of the Othering and Belonging Institute. This foundational concept is why the IDC created the Othering and Belonging Pyramid.
Let's explore the Othering Pyramid, represented in the image above on the left-hand side. It has five parts that include:
Othering and stigma
A lack of ease or difficulty
Not being seen or heard
Experiencing judgment
Unsustainable self-care, behaviors or thoughts
The right-hand side is the Belonging Pyramid. It has five parts that include:
Belonging
A sense of ease
Feeling seen and heard
Nonjudgment
Engaging in renewing and sustainable self-care thoughts, behaviors, and systems
How this diagram can help you.
This Pyramid visually represents how a lack of belonging is the root of many health issues. It also shows how belonging can disrupt stigma and foster a sense of ease, feeling seen and heard, nonjudgment, and self-care.
When our basic human needs for belonging are seen, compassionate curiosity emerges in the following questions.
“What is required in my session or within my organization to create a sense of belonging?”
“In what ways can I foster a sense of ease with my client?”
“How can I help a client feel seen and heard?”
“What can I change in my sessions to support me in remaining nonjudgmental?”
Inclusive Diabetes Care is a weight-inclusive education company.
It offers 12 free foundational courses to untangle the many stigmas in diabetes care.
The Pyramid also uncovers the many ways sustainable self-care is interrupted. It may be due to social and emotional disconnection, a lack of ease, and a decreased sense of safety. It can also include personal behaviors, including fear of speaking or feeling that essential concerns haven’t been heard or acknowledged.
Looking at the barriers to self-care from the lens of inclusion and belonging helps professionals come alongside clients in empathy instead of confusion.
“Having diabetes makes you feel like you can’t belong.”
“You want to have a sense of ease when food shopping.”
“Monitoring your blood sugar isn’t easy at work.”
“Can I ask a few questions so I can hear your concerns about your blood sugars fully?”
“When you went out, you felt judged, which ruined the activity.”
The Cost Of Othering in Diabetes
The American Diabetes Association released the 2023 financial report for diabetes. While these staggering numbers are pointing to cost, it is not hard to see how stigma is an additional cost in diabetes care. The possible stigmas have been added in bold to each finding.
After adjusting for inflation, the direct medical cost of diabetes increased by 7% between 2017 and 2022. - Financial stigma
On average, people with diagnosed diabetes have medical expenditures 2.6 times higher than would be expected without diabetes. Financial, health and diabetes stigma
The inflation-adjusted cost of insulin increased 24% from 2017 to 2022. Financial stigma
Spending on insulin tripled in the past 10 years—increasing from $8 billion in 2012 to $22.3 billion in 2022. Financial stigma
After adjusting for inflation, the total cost of insulin and other medications to manage blood glucose increased by 26% from 2017 to 2022. Financial, health stigma
Despite having a lower prevalence rate, women with diabetes spend more on average than men on annual healthcare expenditures. Gender stigma
Black Americans with diabetes pay the most in direct health care expenditures. Racial stigma
People with diabetes above the age of 65 spend roughly double on per capita annual healthcare expenditures than any other age group above the age of 18. Financial stigma
If people with diabetes participated in the workforce like peers without diabetes, there would be 2 million more people between the ages of 18 and 65 in the workforce. Financial, health stigma
When it comes to diabetes care, sustainable self-care is often tied to the seven types of stigma. These include diabetes, financial, gender, health, racial, and weight. The seventh stigma is unknowing/ignorance, which is not depicted in the graphic below.
How to use the IDC Pyramid: Two examples
Belonging is not just an abstract concept but a practical tool that can transform healthcare institutions by untangling stigma. The IDC pyramid can be used in many ways. For example, it could be used to improve or innovate CX pathways by exploring when customers experience belonging, ease, feeling seen and heard, and nonjudgment. An organization might use inclusion to align business vision and enhance quality measures or patient outcomes. Using the power of inclusion and belonging will make a real difference in diabetes care.
It is easy to overlook the level of disconnection present in society. As noted below, The Belonging Barometer noted that 68% of Americans feel a sense of non-belonging nationally and 74% in their community. For professionals, the IDC pyramid can be used as a counseling framework. For example, verbalizing to clients that they belong during a session is a simple way to foster inclusion.
A majority of Americans report non-belonging, a cumulative term that includes people who are unsure or ambiguous about whether they belong and those experiencing exclusion. Sixty-four percent of Americans reported non-belonging in the workplace, 68% in the nation, and 74% in their local community.
Further, nearly 20% of Americans failed to report an active sense of belonging in any of the life settings we measured, and a small subset (6%) report exclusion across all life settings. These deficiencies in belonging may hold significant costs to individuals, institutions, and our society as a whole.1
Clients deserve diabetes care.
Creating a sense of belonging during the session and allowing our client's lived experience to be part of the appointment is just one way to untangle stigma. This may sound like asking, “What would make caring for your diabetes easier?” or “What changes do you want support to continue?” These simple questions allow the client to feel seen and heard and acknowledge nonjudgmentally the effort they are already making during a session.
The Belonging Barometer: The State of Belonging in America was produced by Over Zero and the Center for Inclusion and Belonging at the American Immigration Council. https://www.americanimmigrationcouncil.org/research/the-belonging-barometer