How To Unlock The Power Of Providing Nonjudgmental Counseling.
The benefits of providing a nonjudgmental approach to diabetes care are endless. But what are the barriers? This article explores the many unseen challenges of nonjudgmental diabetes counseling.
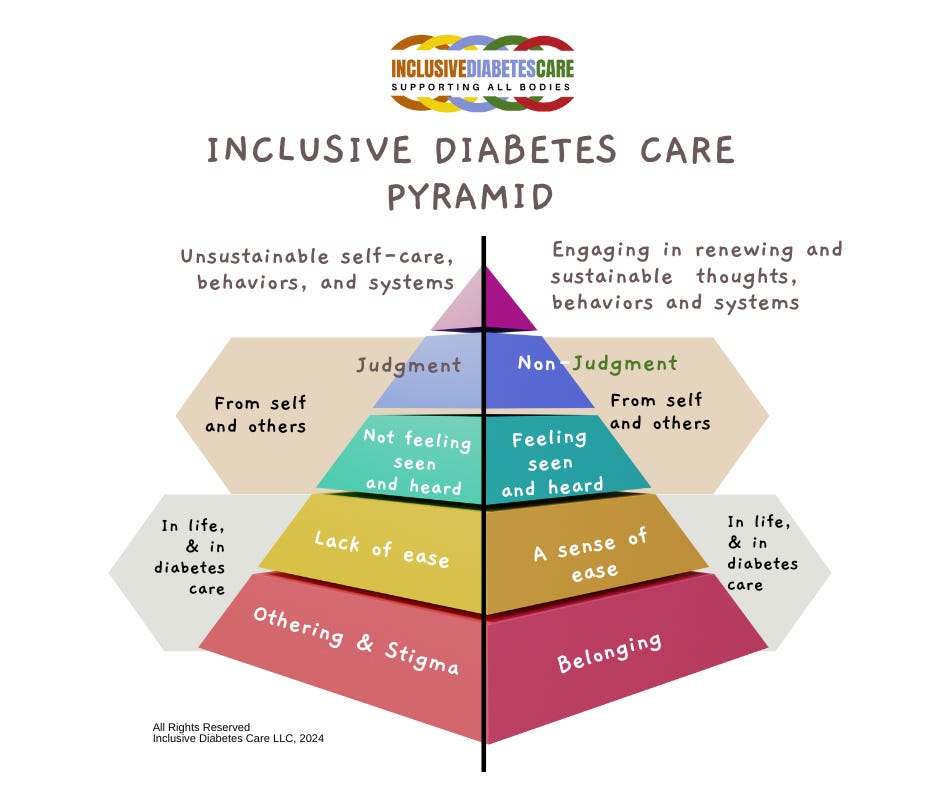
The fourth level in the IDC Pyramid is non-judgment. It is supported by belonging, ease, and feeling seen and heard. Providing nonjudgmental counseling is more accessible when healthcare systems help you, the diabetes worker, challenge the status quo of telling vs. listening.
Welcome to Inclusive Diabetes Care.
The IDC Pyramid is a powerful tool that can help dismantle stigma in diabetes care. This visual representation is transformative and empowers healthcare professionals to see the benefits of inclusion in diabetes care. For a comprehensive understanding, we recommend reading the article Diabetes and Belonging, which provides an overview of the IDC Pyramid.
Understanding how short-term gains reinforce systems of oppression.
From a business standpoint, it is easy to see the appeal of telling clients what to do. Short-term advantages of telling vs listening include simplicity, efficiency, and stating facts, like research supporting evidence-based medicine. However, information alone doesn’t change behavior. Information-laden medical appointments shift the job of process and integrating knowledge to the person with diabetes. When this happens, it lands as another task; it fails to offer support and doesn’t affirm a sense of belonging, ease, and being seen and heard.
Tomesha Campbell, founder of Enhance Black Women's Health Newsletter, explained, “When I feel like I belong, I am given space to ask questions. I am offered an invitation to speak, which is validating.”
A powerful energy is created when people aren’t heard and feel othered. This energy is passed down through stories from generations about previous medical care, family values, and personal experiences. This is the energy of othering. It blends with other forms of oppression, including weight bias, gender inequality, sex discrimination, disability, and racial stigma, to create what Dr. Resmaa Menakem describes in the book My Grandmother’s Hands as “The Charge.”
I learned about “The Charge” during an Education for Racial Equality training. Conceptually, “The Charge” is the collective energy of pain, suffering, and distrust that results from injustice and generational trauma. Unfortunately, when “the Charge” is released, it is believed to be a display of unjust and irrational anger. This description reinforces labels such as “noncompliant,” “difficult,” and “unmotivated.” It inaccurately blames the individual instead of looking to see how and when othering and generational trauma is present.
Let’s use the following example. Imagine a client saying, “I am uncomfortable taking X medication.” A typical response is reassuring the client, saying, “You shouldn’t be. This is safe.” I know I have said it many times. However, it eliminates the sense of feeling seen and heard. It subtly communicates that the client’s fears and concerns are not necessary or valid.
Awareness and Impact of Social Determinants of Health.
Like you, I wanted to understand what to do and how to decrease such interactions. I knew that the Social Determinants of Health are a significant factor in health inequity. However, I needed clarification on how the SDoH intersected with generational trauma and oppression. Luckily, I found the article The House that Racism Built.
This detailed analysis created an analogy to visualize the intersection of SDoH and racism as building a house. In this excellent article, Williams et al. define racism as “An organized system, premised on the categorization and ranking of social groups into races and devalues, disempowers and differentially allocates desirable societal opportunities and resources to racial groups regarded as inferior.” This definition explains that racism is a system. It is the practice of dividing people into groups that “belong” or are “othered,” which is depicted in the left side of the IDC Pyramid.
Next, Williams explains, “Research finds that although socioeconomic status, SES predicts variations in health status within each racial group (i.e., anyone can be poor) that racial disparities persist at every level of socio-economic status.” (i.e., health status was lower in marginalized clients regardless of their income.)
Also read: The Problem with Predisposed
In previous articles, I have written about the health impact of Weathering, which describes how racism, micro-aggressions, and socioeconomic disadvantages put someone under chronic, daily stress that wears down – or weathers – their physical health, leading to accelerated aging and leaving them susceptible to poor health outcomes. When I look at these different variables, it becomes clear that I can’t point to one thing and say, “This is what caused problem X.”
Knowledge and Judgment go hand-in-hand. Admitting my ignorance allows me to express humility. If practiced, it would remind me that I can’t judge what I don’t understand.
Being With vs. Fixing
Inclusive Diabetes Care requires healthcare professionals to have more than a cursory understanding of the SDoH and its impact on diabetes care. This fluidity in knowledge allows everyone in the diabetes space to resist the itch to “fix” the client or situation.
As an individual, I can’t fix historical, intergenerational, persistent-institutional, and personal trauma of racism and intersecting forms of gender, sex, and size oppression. What I can do is listen without blame. What I can do is acknowledge its presence. What I can do is come alongside suffering in empathy. What I can do is identify the systems that maintain health disparities.
Don’t be fooled—this is a very hard thing to do, and the video It’s Not About the Nail will help you understand the more nuanced aspects of how the right reflex manifests in diabetes care. An analysis by Dr Patrick Kingsep, a clinical psychologist in Western Australia, follows this short video to deepen your understanding of the value of non judgment.
Inclusive Diabetes Care also provides professional education about inclusion for diabetes workers. There are 12 courses, with CPE from the Commission of Dietetic Registration.